Wisdom Teeth Removal: A Patient’s Guide
Outline:
1) What wisdom teeth are and why removal is considered
2) Evaluation and planning: imaging, anesthesia, and preparation
3) The day of surgery: step-by-step experience
4) Recovery roadmap: pain, swelling, diet, hygiene, and complication signs
5) Costs, long-term outcomes, and concluding advice
Introduction:
Wisdom teeth, or third molars, are the final set of teeth to arrive, often pushing through in the late teens or early twenties. For many people, they emerge without drama; for others, they cause pain, crowd nearby teeth, or become trapped in the jawbone or gums. If you’re wondering whether removal is right for you—or you’ve already booked a date—understanding the process can turn a stressful milestone into a handled task. The following sections offer a practical, candid walkthrough designed to help you make informed decisions and recover smoothly.
What Are Wisdom Teeth and Why Are They Removed?
Wisdom teeth are third molars that typically erupt between ages 17 and 25, a time when jaw growth has mostly finished. Evolutionary theories suggest our ancestors benefited from extra molars to chew tough, fibrous diets, but modern mouths are often too small to accommodate them. When there isn’t enough room, these teeth can become impacted—partially or fully trapped beneath gum or bone—leading to a spectrum of issues that range from mild discomfort to recurrent infections. Not everyone needs removal, yet many do, and the decision depends on anatomy, symptoms, and risk over time.
Common reasons clinicians recommend taking them out include:
– Repeated inflammation of the gum tissue around a partially erupted tooth (often called pericoronitis)
– Pain, cyst formation, or damage to the second molar’s enamel or bone
– Tooth decay that is difficult to clean or restore due to limited access
– Periodontal pockets and bone loss developing behind the second molar
– Orthodontic or prosthetic treatment planning where third molars complicate outcomes
It’s also possible to monitor wisdom teeth rather than remove them immediately. Watchful waiting is more likely when the teeth are fully erupted, pain-free, and easy to keep clean. However, the likelihood of problems tends to increase with partial eruption, awkward angulation, or proximity to critical structures. Age matters too: in general, extraction is simpler and recovery is faster in younger adults, while surgery can be more involved after the mid-twenties as bone becomes denser and roots fully form. Studies suggest complications like delayed healing and dry socket appear more frequently with increasing age, although individual risk varies.
There are trade-offs to consider. Removal may prevent future infections, assist hygiene, and protect neighboring teeth. On the other hand, surgery involves temporary pain and swelling, time off school or work, and small but real risks such as dry socket, nerve irritation, sinus communication for upper molars, or infection. A thoughtful conversation with your dental professional—grounded in imaging, symptoms, and your preferences—helps balance these factors. The key is individualized planning rather than a one-size-fits-all rule.
Evaluation and Planning: Imaging, Anesthesia, and Preparation
The path to a smooth experience starts with a thorough evaluation. A clinical exam is paired with imaging to map roots, bone density, and nearby structures. Panoramic X-rays provide a broad view of all wise molars and adjacent nerves or sinuses. When a tooth’s relationship to the inferior alveolar nerve or sinus floor is unclear, a three-dimensional scan may be suggested to clarify angulation and root anatomy. The goal is to minimize surprises: knowing how the tooth sits informs the surgical approach and anesthesia plan.
Anesthesia options are matched to your health history, anxiety level, and surgical complexity:
– Local anesthesia numbs the surgical sites while you remain awake and aware
– Nitrous oxide can take the edge off anxiety and enhance comfort while preserving responsiveness
– Intravenous sedation offers deeper relaxation and partial amnesia, with continuous monitoring
– General anesthesia may be considered for complex cases or specific medical needs
Each approach has benefits and considerations. Local anesthesia avoids fasting and allows quick recovery, though you’ll hear and feel pressure. Sedation can make time seem to pass quickly, yet it requires preoperative fasting, an escort, and post-procedure supervision. Your medical history guides safety: disclose allergies, bleeding tendencies, heart or lung conditions, medications (including blood thinners and supplements), and pregnancy. Some medications may need adjustments; always follow the prescriber’s instructions.
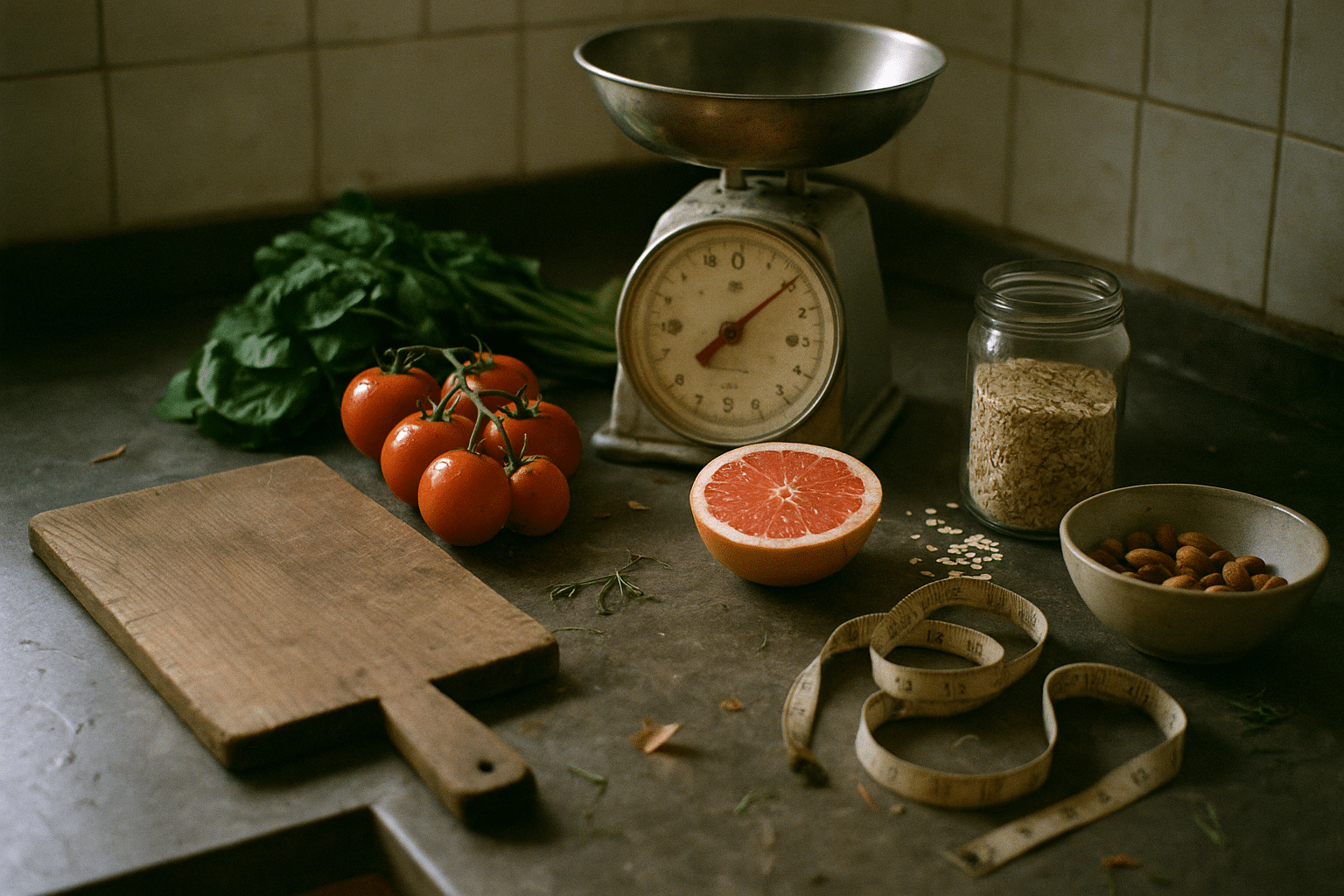
Preparation sets the stage for an easier recovery. Arrange a ride if you’ll receive sedation, and set up a “recovery station” at home with gauze, ice packs, a thermometer, a soft-food plan, and a place to rest with your head elevated. Stock options like yogurt, smoothies without seeds, blended soups, mashed potatoes, scrambled eggs, applesauce, and oatmeal. Avoid crunchy, spicy, or seedy foods that can irritate or lodge in sockets. If you’re instructed to fast, adhere strictly to timing guidelines—liquids and solids included. Wear comfortable clothing with short sleeves for monitoring, and skip heavy makeup or facial lotions so tape and monitors adhere properly.
Finally, confirm details the day before: appointment time, fasting start, escort contact, and any prescriptions. Jot down questions about work or sports restrictions, suture removal, and follow-up. A few minutes of planning now often pays off with fewer headaches later.
The Day of Surgery: Step-by-Step and What It Really Feels Like
On arrival, you’ll review consent forms and medical history, then staff will check vitals such as blood pressure and oxygen saturation. If you’re having sedation, an IV line is placed, monitoring begins, and medications are titrated for comfort. Under local anesthesia, the area is numbed thoroughly; pressure, vibration, and sounds are normal sensations even though sharp pain is blocked. Many patients describe the experience as “odd but manageable,” especially once they understand each step in advance.
The surgical technique varies by tooth position. For erupted teeth, elevation and gentle rocking may be enough to free the tooth. Impacted teeth often require a small incision, a protective flap, and careful bone removal. Sometimes the tooth is sectioned into pieces to minimize force and protect surrounding structures. After removal, the sockets are irrigated and inspected, and dissolving or removable sutures may be placed. For upper molars, the surgeon takes care to respect the sinus floor; for lower molars, the course of the inferior alveolar and lingual nerves guides the approach.
Duration depends on the number of teeth, impaction depth, and anatomy. A single erupted tooth might take minutes; four impacted third molars can take longer. Safety protocols are constant throughout: sterile technique, continuous monitoring when sedated, and readiness to manage bleeding or airway concerns. Complications during the appointment are uncommon, and the team is trained to handle them promptly. Before you leave, you’ll receive written and verbal aftercare instructions and a plan for pain control, swelling, and hygiene.
What does it feel like afterward? Numbness lingers for a few hours, which is a good window to get ahead of discomfort with prescribed or recommended nonprescription medication. Mild oozing is common and controlled with gauze pressure. Cheeks may feel puffy, and jaw stiffness develops over the first 48 hours as swelling peaks. Knowing that these sensations follow a normal arc—up for a day or two, then gradually down—helps set realistic expectations and reduces worry.
Recovery Roadmap: Pain, Swelling, Diet, Hygiene, and Complication Signs
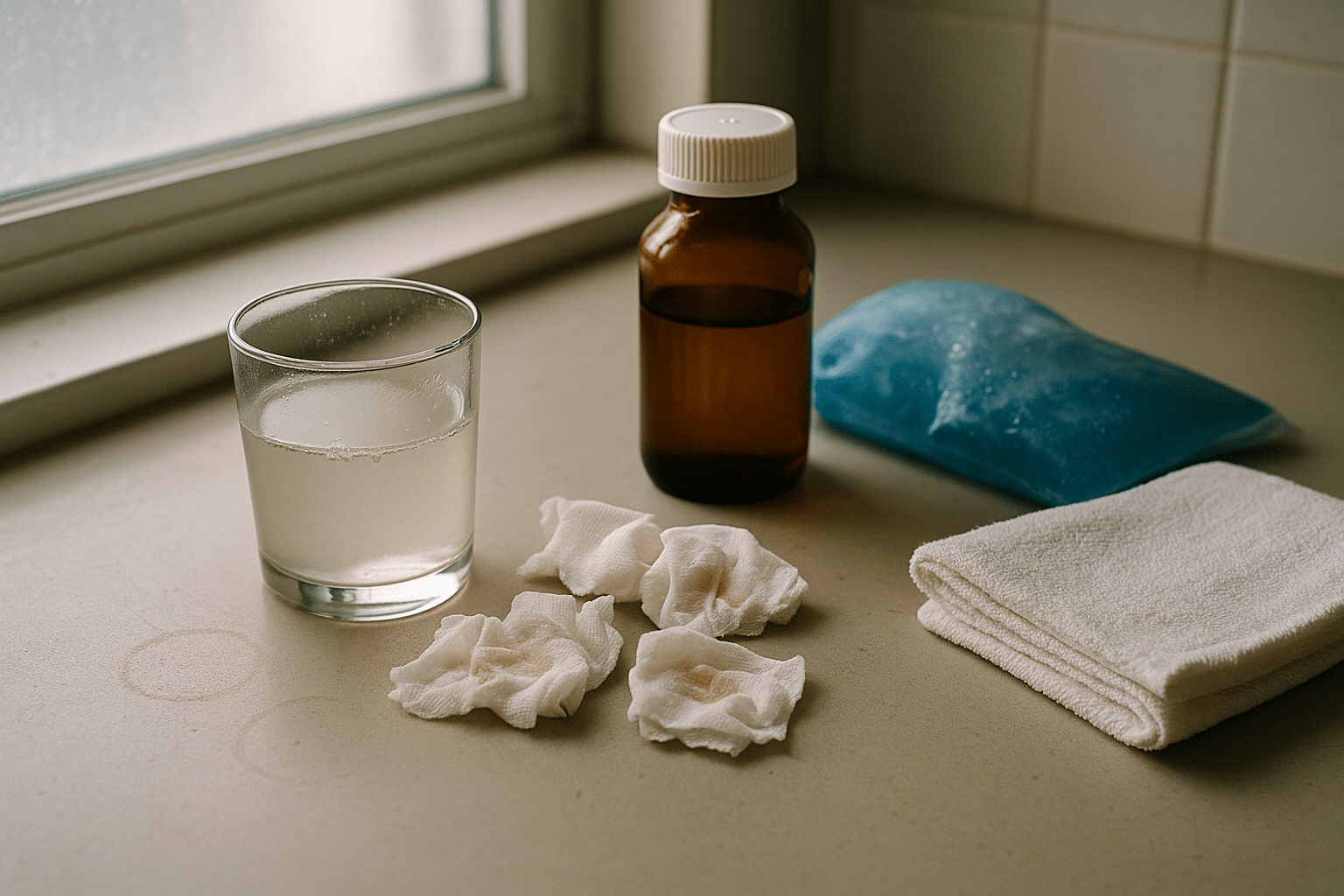
Recovery unfolds predictably, though everyone heals at a slightly different pace. Day 0–1 focuses on bleeding control and comfort. Bite gently on gauze for 30–45 minutes at a time until oozing slows; a dampened black tea bag can help if advised, thanks to natural tannins. Keep your head elevated to reduce swelling, and apply cold packs in 15–20 minute sessions during waking hours for the first 24–36 hours. Many patients find a combination of nonsteroidal anti-inflammatory medication and acetaminophen effective; use only as directed and avoid duplicating ingredients.
From Day 2–3, swelling typically peaks and then recedes. Switch from cold to warm compresses if instructed to improve circulation and ease stiffness. Gentle jaw stretches help with limited opening, but avoid forcing it. Begin saltwater rinses—half a teaspoon of salt in a cup of warm water—after meals and before bed, starting 24 hours post-op unless told otherwise. Keep brushing the rest of your teeth carefully, avoiding the extraction sites until they’re comfortable to approach. Hydration matters, and so does nutrition: small, frequent meals sustain energy for healing.
A soft-food plan reduces irritation:
– Early days: smoothies without seeds, yogurt, blended soups, mashed potatoes, applesauce
– Transition foods: well-cooked pasta, oatmeal, scrambled eggs, tender fish
– Avoid: straws, smoking or vaping, alcohol, spicy or acidic foods, chips, nuts, seeds, and small grains that can lodge in sockets
Bleeding that suddenly increases after seeming to stop can be alarming but is often controlled with firm gauze pressure for 30 minutes without peeking. If the pad soaks quickly more than once, contact the office. Bruising along the jaw or chest can appear after a few days, especially in older patients or complex extractions; it fades gradually. Low-grade fevers can occur early; persistent high fever, foul taste, worsening pain after initial improvement, or swelling that spreads may indicate infection and deserve a call.
Dry socket—when the blood clot dissolves prematurely, exposing bone—produces deep, radiating pain and a bad taste or odor, usually between days 3 and 5. Reported rates vary, from about 1–5% after routine extractions to higher percentages for lower impacted third molars and tobacco users. Prevention focuses on gentle care: no straws or vigorous spitting, excellent oral hygiene around (not inside) the sockets, and avoiding tobacco. If it occurs, in-office treatments can soothe and speed relief. Nerve changes like tingling or numbness of the lower lip or tongue are uncommon; most resolve over weeks to months, and persistent symptoms should be evaluated.
Plan your return to activity thoughtfully. Many people resume light work or school within 2–3 days; strenuous exercise, contact sports, and wind instruments may need a pause of 5–7 days or more depending on swelling and comfort. Driving is off-limits the day of sedation. Build rest into your schedule, and don’t hesitate to ask for a tailored note for school, work, or athletics if needed.
Costs, Long-Term Outcomes, and a Patient-Centered Conclusion
Financial planning helps avoid surprises. Fees vary by region, provider training, number of teeth, impaction depth, and anesthesia type. A straightforward removal under local anesthesia generally costs less than an impacted extraction with intravenous sedation. Insurance coverage—if available—may distinguish between medically necessary and elective procedures, apply annual maximums, and handle sedation separately. When you request an estimate, ask for a breakdown that includes consultation, imaging, extractions per tooth, anesthesia, potential pathology evaluation, and follow-up visits. You can also inquire about payment plans or timing care across benefit periods when appropriate.
Long-term outcomes depend on both the original anatomy and the quality of care during recovery. Removing problematic third molars can reduce recurrent infections and protect the second molars from decay or periodontal defects that are difficult to repair later. For symptom-free teeth that are fully erupted and cleanable, observation remains a reasonable path with periodic imaging. The decision is nuanced:
– Pro removal signals: recurring pain or swelling, decay that’s hard to treat, cystic changes, damage to neighbors
– Pro monitoring signals: asymptomatic, fully erupted, easy to clean, minimal risk on imaging
– Patient factors: age, medical conditions, tolerance for potential future surgery, access to follow-up care
It’s helpful to separate myth from reality. Third molars are not the sole cause of dental crowding; orthodontic relapse can occur even without them. Not every impacted tooth turns into a cyst, but the chance is real enough to warrant periodic checks. Surgery is not universally “easy,” yet with planning and good technique, most recoveries are predictable. Your experience is likely to be shaped by preparation, clear instructions, and steady self-care in the first week.
Conclusion for patients: you have options, and you’re in charge of the plan. Start with an honest evaluation that matches your anatomy and goals. Choose an anesthesia path that fits your comfort and health. Prepare your home with soft foods, ice packs, and a quiet corner to rest. Follow the recovery steps and listen to your body. If something feels off, reach out promptly—early guidance prevents small concerns from becoming big ones. With realistic expectations and a simple checklist, this rite of passage becomes a contained, manageable chapter rather than a daunting story.